Guillain Barre Syndrome Neurology
DISEASE OVERVIEW
• Group of autoimmune syndromes consisting of demyelinating and acute axonal degenerating forms of the disease
• Rapidly evolving polyradiculoneuropathy preceded by a triggering event, most often an infection
• Incidence: 1 to 3 per 100,000 persons annually
• Campylobacteriosis is the most common precipitant in GBS
• Influenza vaccine is associated with a risk of 1-2 cases GBS per 1 Million
SIGNS/SYMPTOMS
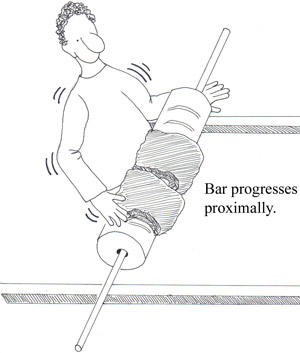
• Progressive, symmetric neurologic symptoms
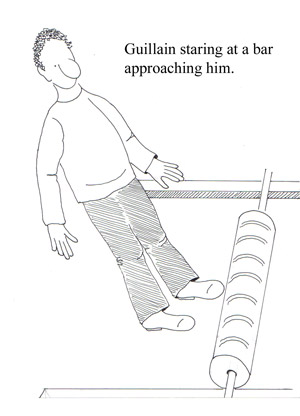
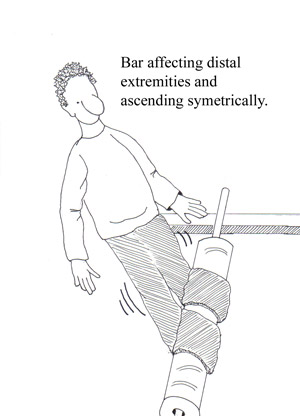
• Weakness (proximal muscles; legs more often than arms) see figures below
• Tingling dysesthesias (extremities)
• Paresthesias (spread proximally) see figures below
• Disappearance of deep tendon reflexes (within the first few days of symptom onset)
• Cranial nerve involvement may affect airway maintenance, facial muscles, eye movements, and swallowing
• Pain (shoulder girdle, back, and posterior thighs) See fig 3 below
DIAGNOSIS
• a definitive diagnosis is usually not possible until the fifth day after the onset of symptoms
• Clinical features: progressive weakness in both arms and legs; areflexia
• CSF findings: elevated protein (greater than 0.55 g / dL ) without pleocytosis
• Electrodiagnostic findings: an absent H reflex, low amplitude or absent sensory nerve action potentials, an abnormal F wave, and other less frequent abnormalities
TREATMENT
• All patients who have GBS should be admitted to a hospital for close observation for respiratory compromise, cranial nerve dysfunction, and autonomic instability
• Monitor lung function
• Physical therapy
• Pain control with narcotics along with carbamazepine or gabapentin
• High-dose intravenous immunoglobulin (IVIg; 400 mg per kg daily for five days)
• Plasmapheresis (five exchanges over five to eight days) OR IVIG
- Anatomy
- Anesthesiology
- Cardiovascular Medicine
- Dermatology
- Emergency Medicine
- Endocrinology
- Gastroenterology
- Geriatric Medicine
- Gynecology
- HIV
- Hematology and Oncology
- Infectious Disease
- Internal Medicine
- Nephrology
- Neurology
- Obstetrics
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pediatrics
- Pharmacology
- Prevention
- Psychiatry
- Pulmonology
- Radiology
- Rheumatology
- Surgery
- Urology
- case report
- trial reference




